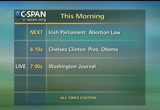
tv News Politics and Public Affairs CSPAN January 20, 2013 3:00am-6:00am EST
3:00 am
5:00 am
we do have excellent remake of psychiatrists. we only have three. but we are not talking about dealing with all issues pertaining to mental health. we are talking about the tiny number of women who wish wish to kill themselves during pregnancy. that is a tiny number of women, i believe we have the capacity to that. -- to do that. it must be stressed, we are talking about small numbers of women. very interesting question about the substantial risk to life. how is that incest. -- how is that accesassessed.
5:01 am
those who might take their lives. we never will be able to come up with perfect legislation or regulation. we are asking for lawyers to draft legislation that allows for flexibility. it would be impossible to write a list of disorders which might qualify. that is not what i am asking. i believe that to expert medical doctors or additional doctors in a variety of specialties, for example cardiologists, to obstetricians who are experts in the field, who are able to gain the information they need, obtain advice from their colleagues, two consultant obstetricians are able to determine when there is a significant risk to life in a pregnant patient. i believe they should have the ability and flexibility to
5:02 am
identify those women and treat those women appropriately without fear of prosecution. it is a medical decision, whether or not someone is likely to die. it is a medical decision based on medical fact. doctors must be able to make this decision if they are to do their job properly and preserve life. thank you. >> thank you. >> thank you. i would like to echo all of the comments that the dr. has answered. how do we impact -- what is the impact of legislation if we do bring in legislation, which allows termination of pregnancy in this country? what will the impact be on our services? i do not think we know the
5:03 am
answer to that question. i would agree that risk of death and suicide is extraordinarily rare. however, we do not know the number of p o -- people who go from ireland to the uk, seeking termination of pregnancy and that there's -- in that jurisdiction. we do not know the answer to that. there are people who seek termination of pregnancy because of rape, incest, because they have debuts with lethal abnormalities. some of those women will come to us and have significant mental health issues. those women will need to be assessed by site 3 -- by psychiatric services. there will be an impact, but we do not know how big or small it is going to be. in terms of conscientious objection, i cannot think of any
5:04 am
circumstance where any health professional and a mother's life at risk would say that they would not be involved in her care. i can't see that would be an issue. if the mother -- if her life is genuinely at risk. in terms of legislation, it needs to be -- it needs to have a flexibility to have the medical profession to make appropriate decisions. i think we need to trust our medical practitioners to make the appropriate decisions. the regulation that is put in place has two inshore that there is an appropriate number of suitably qualified doctors who make the decisions, and they need to be protected by legislation. as termination of pregnancy
5:05 am
ever necessary? i would say yes. and our hospital, last year, we had six situations i can absolutely tell you for sure that if intervention had not been made, then that mother, if she had not died very soon after the event, then she would have died subsequently. then i would say yes, the situations do happen. in our hospital, they happened six times in the last year. if i have not answered all the questions, please come back to me. >> ok. to the deputies question about should list be published? i have huge concerns with publishing most. doctors will manage patients on a case-by-case basis. every case will be different. there is always a risk that if you publish lists of people who will do a, b, and see, you will
5:06 am
be discriminating against people. the important thing is, no practitioner will ever allow a woman to die because they will not do something. we are there to save lives. we do it all the time. the deputy asked about legislation impacting us. the life of a mother has always come first. yet, pregnancies have had ended earlier than anticipated because the life of the mother was at risk. about cancer, i would feel terrible even talking about cancer. i have had patients who have had cancer and had appropriate treatments, surgical treatment in pregnancy who have gone on to have chemotherapy at a later stage in pregnancy. radiotherapy after pregnancy is completed. it is a case-by-case basis.
5:07 am
it is about communication. dealing with the mothers life life is what is most important. there may be situations where a baby will be delivered early because the mother's life needs the treatment. more and more cancer services -- the evidence is showing that you can get to a point in the pregnancy where the baby is viable. that is what we are always aiming for. in terms of the suicide issue, we need to become very focused on the fact that there are other treatments for suicide. if a patient said he wanted to kill himself, there would be medical treatments, drugs, therapies, and they would be reviewed in a couple of weeks. cases are reviewed after a couple of weeks. the questions mainly -- >> eight speakers now have indicated -- if members could
5:08 am
be brief and their questions in response. >> thank you. to connect think each of the speakers further presentation. first, -- i want to thank each of the speakers for their presentations. in the rotunda, five to six in the last 12 month. , terminations. is it likely that there will be a higher rate, because it is a referral hospital? any indication of the type of numbers we are talking about? secondly, you made the point about one and -- in half a million women present with suicidal tendencies. has there been any research in relation to where a termination takes place, whether it has
5:09 am
increased or reduced the suicidal tendency, or does act as a cure to that tendency? is there any research in relation to that whatsoever? you make the point that there is a need for a pathway to be put in place for decision-making in cases of smaller hospitals. i want to thank the doctors for being here. if i can refer them back to the evidence we received earlier from the medical council who said that there should not be specific provisions for emergencies. but you, dr. mccarthy, specifically talked about emergency situations where you make the point that in relation to the second opinion it should not be a physical -- in an
5:10 am
emergency situation. can you comment on what the medical council has given to us here? i would like the view of both doctors in relation to that. could you also count -- there is a genuine fear among people that this could be constructed in such a way to reduce the capacity of some of the smaller maternity hospitals. >> thank you deputy. >> thank you to our expert witnesses. one of the things to me is the lack of certainty, whether a woman's life is absolutely at risk. i very much feel for that, because my wife had very difficult pregnancies. my question really relates to
5:11 am
this, if we are to legislate adequately, is it possible to do so without going back and removing the article in our constitution which puts restrictions on abortions? >> deputy shamus. >> i would like to thank the witnesses for their testimony. it has been helpful to me. a number of issues. the probability of substantial risk to the life of the mother. i would just like some clarification in relation to that. we all understand an immediate situation. would there be a situation where the life of the mother might be at serious risk down the road, six months, 12 months, two years?
5:12 am
also, the question of local units and emergencies was raised earlier. it was probably not done effectively, in my view. dr. mccaffrey, your submission suggests that the local units would only team as emergencies, the other issues would be in the activated in cork and galway,, is that what dr. mccaffrey is suggesting? in relation to emergency, the medical council suggests there is no particular procedures are necessary in relation to this. i wonder you on that. and in relation to conscientious objections and in her --
5:13 am
conscientious objection, it is not always absolute. i take it from what people have said that that is the first to specifically case of emergencies. >> thank you. >> thank you for coming in this morning. against the backdrop of describing the level of medical care and intervention, i think that is a given. you said particularly that there was something that was stopping you from making sound medical judgment and decisions relating to medical care of women. let me ask you what that something is, given the clarity of the medical guidelines discussed earlier. also, to all of our guests, can
5:14 am
i ask how many terminations or early deliveries have taken place in your hospitals? >> thank you. we have already established that if i stand up, the microphone does not work. please do not see any disrespect. i would first of all it to thank you all, but i would like to also commend you. you have all made me a little prouder to be a dr. today. rate clarity, honesty, and conviction in what you have said, and i think that is critically important. i am sorry, we must seem like we are wasting time. extrapolating from a just proportionate number of complex pregnancies in dublin, i am guessing that nationally we
5:15 am
probably have something like 30- 40 terminations of pregnancy which are necessary and are now carried out to save the life of the mother? erect me if i am wrong. -- correct me if i am wrong. also to clarify, i'm not hinting at anything specific or asking anyone to put themselves in a position to stand in judgment of their colleagues, is it any of your opinions that there have been maternal deaths in this country which were needless, unnecessary, and which would have been specifically invented, had there been greater clarity in the framework? the termination of pregnancy was not offered, because the dr. felt that he or she was not adequately, legally covered, or might have been breaking the law if they performed it. i would also ask to touch on one other issue which is being
5:16 am
mentioned in the other house of parliament. that is the distinction between a termination which is necessary to specifically save the life of the mother, as opposed to for the health of the mother. because that is being advanced. my own sense, i may be being medically naïve, but there are conditions that threaten your health, but to a small extent threaten your life, and as such, it is probably not a huge issue. i would also like to ask you to clarify, -- sorry we will not be going into medical details. is it ever necessary in performing a life-saving termination of pregnancy, to specifically kill the fetus in utero? or can the pregnancy be delivered to give the life- saving indication which the woman needs question mark i know this is something that others have raised in objection.
5:17 am
also to clarify something from earlier, a hospital in the u.k. where the anesthesiologist refused to anesthetize the patient -- i am sure you meant not in the case of emergency? thank you very much. >> it is probably better if i sit because of the microphone. i think the number of terminations that we would perform in the hospital last year was six. it is my belief that the number would be roughly similar, but the incidence has risen in recent years. i think the reason for that is possibly due to the increasing
5:18 am
age of the pregnant population. the increasing complexity of illness. also the rise in obesity levels. i think they have all come together to increase the risk for our population. in terms of risk of suicide, when i said one in half a million, that is the incidence of suicide in the population, not the incidence of people coming forward with suicidal ideation, which would be a lot higher than that. in terms of certainty of risk, it is hugely difficult and area. there are many gray areas. i think that we need to trust in our medical practitioners. we have a fantastic quality of health professionals working
5:19 am
within our health service. the problem is getting in to see them. we have to trust in our excellent doctors, trust in the judgment of those individuals and protect them in making those decisions. do we need to review or change or take the existing laws of the statute books? i am not a lawyer, so i would leave that question to the lawyers. have we ever had to perform a termination of pregnancy because of risk of suicide? not in my experience. senator, you asked the questions about the numbers from the rotunda nationally. i think he is in the right ballpark. he would probably see more of these complicated cases. i would have thought that the
5:20 am
figure nationally is probably 20-30. but you are in the rate region. -- right region. have there been any needless maternal deaths because people felt that they could not or would not act? i am not aware of any such tuition. -- situation. the situations where a fetus needs to be killed in utero rather than delivered? in most situations, it is possible to deliver the baby or fetus without actually killing the baby in most situations. >> thank you. >> i think they need to stand. in terms of maternal deaths because of needless of detrick intervention -- i am not aware of any, either. i am not aware of any deaths as
5:21 am
a result of suicide because a termination was declined to somebody. in terms of deputy heelys questions, i thought i made it clear that the more severe medical cases like cardiac disease, we would be sending those out to be managed by multidisciplinary teams in a different unit. it would almost always be dublin. the obstetric emergencies, we manage in smaller units. three-man units vary in size. it depends on the skill mix. it depends on who you have on duty on the day. it depends if there is an intensive care available to you. that is why the expertise of the clinician at the end of the bed
5:22 am
has to be a knowledge. it has to be protected in law that they are making the right decision for that patient at that moment in time. we have to look to the track record of smaller hospitals. we have a very good track record in how we manage our patients. sending out appropriate patience and managing patients locally. in terms of the second signatory, i know the medical council have said it is not necessary, i think it is good practice to discuss very complex cases with a second person. a lot more things go wrong when you have local staff on duty. one of the process -- proposals i did not get to talk about was a place for looking about having a panel of experts nationally, if they are not on duty, they usually have a deputy. that we would have resources to
5:23 am
fall back on if you needed to discuss a complex case and come to a conclusion. you hope it would never happen, but what if the second colleague in your hospital did not agree with you, can you would have to take it to a higher level to get to the opinion of another person. you have to look at strategies to deal with his news. in general, our track record has been good. >> thank you. >> back to the idea of suicide. yes, the incidence of suicide is trim the rare. this is not the same thing -- extremely rare. this is not the same thing as the ideation. it would be difficult for anyone to identify what is the instance of suicide. often these cases are returned in the corners courts as open verdict. we can say with some certainty, it is rare.
5:24 am
some women would take themselves to a different jurisdiction and choose to terminate their pregnancy. it is extremely difficult to assess what is the true instance of suicide. coming back to the whole issue surrounding lack of certainty, there will always be one because of medical probability. the assessment of the risks to life in the context of medical disorder is a medical decision. doctors must be trusted to make these decisions. this is our area of expertise, this is what we do. what we're asking for is that we are legally protected in doing this job. to be specific in the way that i feel is a block -- i feel -- i take issue with section 58 and 59, i think it is a problematic
5:25 am
area. i think that needs to be addressed. in terms of extrapolating cases -- how many extra cases of termination of pregnancy do we anticipate? in my hospital last year, we had three cases where we had to intervene higher to fetal viability because of our concern that a woman would die. a tiny number of cases. i think 30-40 is an overestimate. i imagine it would be more like 10 or 20. these numbers are very tiny. we never kill a fetus. that is not what we are about. occasionally it is required that we deliver a pregnancy before the baby is viable.
5:26 am
or capable of surviving and neonatal intensive care. i would like to reiterate that when there is any chance, any possibility that we are able to preserve the life of the baby, we will do so. we are able to do so from very logisticians, 23 weeks on. we will make every effort to preserve life. other cases where we are required to terminate, not killing the baby, that is delivering the baby before it is ready. 1.i would like to address is the changing demographic. older women becoming pregnant. it is very important that doctors have the flexibility to do their duty with legal protection. thank you. >> our next figure is the
5:27 am
deputy. >> thank you for being here this morning. i hear you loud and clear. you are saying, let me do my job and let me be protected. that has come across very clear. i am a mother of five children, and i have had my own misfortunes of miscarriages. it is a great joy when you are told to pregnant and then things happen and do not go the way you would like them. the honesty and trust that you have in the maternity hospital, that is very important for all of us. i want to refer to something i raised this morning with the medical council. section 21, just around this, it
5:28 am
is long. due to extreme immaturity of the baby, there may be little or no hope of the baby surviving. in these exceptional circumstances, it may be necessary to intervene to protect the life of the mother. making every effort to preserve the life of the baby. my cells and other colleagues -- myself and other colleagues -- people still having to leave this country and having terminations of pregnancy. a lot of them are due to the extreme immaturity of the baby. having to bring back the dead baby in a box or car. " made it at home. -- cremate it at home. according to this, what i have
5:29 am
read, correct me if i am wrong, does this not mean that we should not be sending the way those people when do know as professionals that these people, the circumstances that they are carrying their baby that they are not going to live? there are a lot of women out here. a lot of women experiencing these difficulties. stories of people having to go away. maybe you could clarify that. >> thank you. >> thank you very much for your presentations. can i go back to the presentation this morning from the medical council. i cannot seem to get it. they said explicitly this morning that special procedures do not need to be developed for emergency situations. i would like to comment. are you in agreement or not with the medical council?
5:30 am
we are here trying to accept information. and work on it. i just want to ask you, you talked about -- i would like to know what deficiencies are in the medical guidelines there at the moment? the third point is about the hospital. does it impact different hospitals and how women are treated? thank you. >> to questions. pregnant women get into treatment -- [indiscernible]>>
5:31 am
first of all, to address women in ireland to face the threat of dying during their pregnancy not only require compassion and understanding, but i would argue that they require good, sound, medical treatment. we must be able to treat them within this jurisdiction. it is always all about appropriate medical treatment. based on medical circumstance. in regards to the medical council, a specialty is not required. generally speaking, an emergency situation, we are talking about a woman who might be actively hemorrhaging and might be about to die. of course there is not time to have any sort of negotiation
5:32 am
about what is the right thing to do. we simply treat that woman. hospitals who practice obstetrics have the backup to do that. we always have an obstetrician on call, and a second one on back. an emergency situation where a woman is dying, i believe we have the resources to manage those. we do so without hesitation. in terms of needing care -- i still contend that as a dr., i need further clarity that i am protected within the law. as i have said, the 1861 defenses against the person act 's tilt stands. the supreme court's judgment has not been legislated for, even though it is over 20 years since that judgment. it is open to a degree of interpretation. it is not supported by legislation. please be real short, we are asking for legislation that is
5:33 am
broad enough to allow us to do our jobs, but we also want regulation. we want this process to be monitored. in all of our opinions, i believe, we need board legislation to allow us to do our job. this should be regulated in the patient's interest. society can be sure that we act appropriately at all times, and only to save the mother's life. it is part of all the steps but for that we would monitor terminations of pregnancy in order to save a life. we can be very clear that all decisions to do so are appropriate and according to the wishes of our society, to reserve life. we are about saving women's life. it is not about terminating pregnancy or destroying babies. it is about saving women's life. the cost of the hospital, we do not practice according to any we practice according to the
5:34 am
demand and clinical situation. it is very difficult for us to set whether or not the number of lives we might save in this scenario would introduce termination of pregnancy and believe we are saving lives. a woman is actually dying in front of us, but it is the cases that i argue that the risk of life may be delayed. the woman with cancer. a woman with serious underlying disorders. any of these women travel quietly to other jurisdictions where they terminate the pregnancy. that is a fact. they are among the 4000 women who travel from this jurisdiction every year to terminate their pregnancies for whatever reason. it is very difficult for us to
5:35 am
assess the negative impact of not having the policy to terminate safely when the risk to life might be delayed. we need to be able to do that when it is necessary. i cannot sure you, the circumstances are extremely rare. but they do exist. doctors are simply looking for the adequate protection to make proper decisions to save others'lives, nothing else. this is a very narrow, confined concept. >> just to address the issue of special circumstances, i think with the medical council was saying was that you did not need a second union or signatory or process in place to actually carry out an emergency procedure. if someone is bleeding in front of you, and her life is at risk, you get on with it. >> start again, please.
5:36 am
>> with the medical council said this morning was that you did not need special procedures for emergencies, or second signatories. we are very different in a smaller hospitals. we do not have a second on-call obstetrician. what people want is that the legislation be couched and worded in such a way that we would be protected. that we will not end up in prison because we did something and someone decides that we should be reported to the medical council. it is a huge fear among people because it is an extremely emotional profession. we practice with clinical guidelines. they are there from us from the college of london. people practice what is in the
5:37 am
best interest of patients on evidence. >> i don't think that i have anything new to add to what has already been said. the answers to those questions. there are a substantial number of women who travel to the u.k. for terminations of pregnancy because of anomalies. that is regrettable that that situation exists. i think the discussion is not around that particular area that may be a discussion for a different day. emergency intervention -- the medical council guidelines are there. aat we're after here is change in legislation to protect doctors and performing life- saving tasks that they have to do. i would entirely agree with
5:38 am
what has been said about hospitals. we have evidence-based practice in this country. guidelines from our own institute and from the royal college in london. i do not think that is a huge issue. >> seven minutes remaining. be very brief, please. >> coming back to dr. mccaffrey 's evidence and medical emergencies. we did question this morning the medical council of london. he said there is a need for special procedures for emergency situations. that does not mean there is not a need for a second signatory. the impression we got, it was hard to get a straight answer, was that there should not be any differentiation between an
5:39 am
emergency and a nonemergency. the same procedure should apply. in that instance, if a second signatory was required, how would that apply in an emergency situation in a small maternity unit? >> i understand if you feel unable to answer the question, it is more of a legal question then medical, but if you are willing to hazard an answer, i would appreciate it. just to follow-up on the instances, accepting the statistics in relation to a situation where the woman's life is at risk on medical grounds and the even rarer situation where there are suicidal ideation but intent, can you clarify your view as to whether or not the rarity, particularly
5:40 am
in the latter, is a reason not to legislate? not to regulate? my view would be that if there is the possibility presenting that there is an onus and responsibility. lastly, as is when the benefits of this engagement, you highlight the situation of the women's hospital, dealing specifically with medical problems in pregnancy, would you like to offer any other view? are you commending that clinic for replication across the network? >> please be concise. >> that is quite a long question. he has given me an inning to say what i want to say.
5:41 am
if you look at the report from the u.k. that looks at mortality -- maternal mortality , there is a real need for a specialty that they call obstetric physicians. general physicians with an interest in pregnant women and their illnesses. that model of care has been rolled out in the uk. there is no official structure, but there is a need for that kind of specialty. i hope that we would minimize the need for people getting to the point where they are in situations that they are faced with now. i am commending the model, and i think it is worth the fighters and to look at in the future. i am a bit unclear about the
5:42 am
rest of the question. >> the medical council said that there should not be a differentiation in the legal framework regarding emergency and nonemergency termination. in a smaller unit, or you have only one consultant available, and there is a requirement for a second sign up in an emergency, how do you deal with that? >> the medical council had their opinion, and i understand that. we have the opinion that you do not need a second signatory. if there is legislation and regulation that determines that we need a second signatory, then a process will have to be put in place for the smaller hospitals to allow that to happen. in my opinion, it would be asked provided by having a panel of experts or peers that we
5:43 am
would be in a position to ring and get that second opinion. e-mail, skype, do all sorts of things. it will have to be looked at. women will continue to be delivered in the smaller units. there is no reason why they cannot be. >> very quickly, in terms of emergency, this is a pragmatic thing, we must save the woman's life. she is dying in front of me, i will not wait for a second signature. i will save her life, that is my job. in terms of suicide, i do not believe we should dismiss suicide as a potential for a woman to take her life during pregnancy. to do so would be judgmental, it assumes that women would lie and fabricate suicide ideation which offends me. it assumes psychiatrist in this country are unable to assess suicidal ideation. i do contend that suicide ideation is extraordinarily
5:44 am
rare. it is extremely rare. it must not be confused with general issues surrounding mental health. >> thank you. i hope that we have been straightened -- demonstrated that there is a requirement for legislation in this area. life-saving procedures do occur. they do not occur often, but they do occur. we do procedures that require interruption of pregnancy. therefore, we need protection of our doctors for these procedures. in terms of maternal medicine clinics, they do exist. they are a fantastic multidisciplinary care set up. they provide best practice care for our patients. they should be rolled out to every maternity unit. >> thank you.
5:45 am
that concludes the session. there are five members who have indicated -- two minutes. >> thank you very much. witnesses, thank you for your clarity. dr., you spoke about the legal uncertainty in very narrow, rare situations where the mother's life may be saved by a termination. we now have to frame legislation. what should the parameters of this space be, that narrow situation that you have described? and how i -- how might we describe it? it second, you mentioned interpreting risk. he said the mother see you and should be taken into account. these hearings are not hearing from any mothers who may have been in this situation, where they may have been advised
5:46 am
abortions. i was struck by the fact that you said we never kill a fetus. sometimes baby are born alive after abortion procedures in other countries. what do you think would be an appropriate response to this, under the proposed legislation? is there a duty of care in these situations. finally, you have had six terminations to save a woman's life in the last year. senator crown mentioned this as well, but i am not clear on the answer? are you aware of any situation in ireland where medical treatment may have been withheld on the ground of lack of legal clarity, and is there a possibility that it may not have been reported because of that lack? >> just want to ask dr. mahoney
5:47 am
quacks have you ever withheld treatment or refused intervention to save the mother's life on legal grounds? is there any evidence that pregnant women do not receive appropriate medical clear in the current state of the law? a difficult question, i think it is critical that we have all the facts. in relation to the patient who is suicidal, exactly what is the procedure in which the pregnancy would be terminated? for instance, if she is 24 weeks pregnant, what exactly would you do? what is done to the baby in this pursuit or, what is done? also, are there any constraints in carrying out abortion in the
5:48 am
later stage of pregnancy, where a woman resents thoughts of suicide. the dr. constantly refresh -- referred to a patient, did you not think that were to patients question mark mother and baby. >> first, she mentioned that one in half a million commit suicide. do you have the statistic for the number of pregnant women who present with suicidal ideation. one and a half million, over what. ? over recent years, a month? it is difficult to obtain information on this. dr. mahoney, you welcome the legislation and regulation, but can you clarify what legal protections -- is that supposed
5:49 am
a clarity of procedure that you require the legislation. do you believe that legislation regulation can provide greater clarity of procedure and the current medical council guidelines? have the guidelines invented you from saving the life of a mother in the past, and if so, how? i note you are a member of the institute of obstetricians and gynecologists, and how has the institute handle changes to those guidelines? >> [indiscernible]>> 24 weeks, we do not anticipate termination of pregnancy at 24 weeks. when there is an opportunity to save a baby's life, we will do that.
5:50 am
somewhere around 23 weeks gestation we would expect a chance for survival. we will offer a baby every opportunity to survive. neonatal and intensive care. let's not ever talk about termination of pregnancy at 24 weeks. we would deliberate baby, who maybe has a good chance of survival. probably over a 90% chance of survival. let's not confuse this issue. without treatment -- i have not. i do not feel legally protected in this country in delivering appropriate medical care and all cases. people ask me about the legal uncertainty. 1861, the act that remains law in this country. what we have is the judgment of the x case that allows for the termination of pregnancy that
5:51 am
includes the risk of suicide. but that has not been legislated and is not supported by legislation. i can see no reason for not doing so. in terms of legislation, i am not a lawyer, but what we are looking for is that the flawed legislation would allow us to do our job. dashboard legislation to allow us to do our job. as medical expertise improves. we may require to fine-tune the legislation. legislation should be broad. the 1861 at 10 commit a woman and her dr. to prison. doctors deserve legal protection.
5:52 am
i will finish there. >> i am not aware of any situation where lack of legal clarity has prevented appropriate care. it has not happened in our hospital. i have never withheld the appropriate treatment for a patient when it was required. in terms of the risk of suicide, i think that all of the appropriate mental health support need to be made available for women who are at risk of suicide. most people would agree. you can ask the psychiatrist later on. most would agree the termination of pregnancy is not a treatment for suicide. i do not have the numbers for the u.k. or for ireland in terms of the numbers of people who would have suicidal ideation.
5:53 am
the one in half a million pregnancies were suicide has actually happened comes from their most recent report. >> with regard to treatment being withheld because of the law, i am not aware -- i never withheld treatment. i have never heard of it from a colleague. i think women receive appropriate treatment. with regards to the suicide issue -- i have exhausted my limited expertise. the site -- the psychiatrist will be enlightening this afternoon. i am sorry if i offended anybody by mentioning patients and not baby. loosely using the term patient to refer to the person with the illness or condition. >> thank you, chairman. briefly, could i ask the
5:54 am
speakers who mention suicide and it is rarely used as a reason for termination. could i ask you, are there mental health issues in your opinion, on mothers who lose their babies, or the baby -- as a result of losing the baby? is that very rare as well? how does it compare with the figures for the mothers who might want termination because they are pregnant? >> senator. >> three brief questions. first, thank you for the clarity
5:55 am
with which we got answers. the evidence before the court was that the woman had been undergoing chemotherapy for three years. then she went into remission and became unintentionally pregnant. can i just ask, in those circumstances, another woman presenting herself to you in the circumstances, what treatment would you have afforded her in that position? my second question, probably to dr. mahoney, you need -- expressed the need for legislation. how should legislation be designed and what impact might it have on current medical practice? underpinning current medical practice the satisfactory o? if you could give clinical
5:56 am
examples in your answer, it would be helpful to us. my final question for the offense against the state act. any changes or any repeal of the act should also -- should the baby also be afforded some protection and law? >> thank you. >> thank you chair. i would also like to thank the witnesses. really strong presentations. i really chilling effect of the 1861 acts on current medical practice. you have really testified to that. i just wanted to ask him a a specific restaurant about the drafting of legislation. -- i just wanted to ask a
5:57 am
specific question about the drafting of legislation. in nonemergency situations, to opinions -- should it be to obstetricians? one obstetrician, one other dr.? should it be a psychiatrist? weigh the disadvantages, not quite clear. it seems to me they are coming down on the side of an obstetrician plus one other. that would be the normal process. >> most of my questions have been asked. final question, from the three professionals that have given their presentations today, would that be representative of their professional colleagues, or are there those in the group that has many different views held? >> senator, you indicated --
5:58 am
>> for dr. mccaffrey. you spoke about consulting colleagues around the country. 280 years of experience and you were unable to identify any consultant who met a woman wishing to terminate identity due to suicide. -- terminate pregnancy due to suicide. is this in other jurisdictions where abortion is legal? >> having practice abroad in all of their experience, they have not met a woman who had suicidal intention or ideation purely because she was pregnant. that was just a group of 12 consultants. with regard to the two signatories, the people i spoke to, nobody thought it was
5:59 am
appropriate for obstetricians to have an opinion on suicide. without that was for psychiatrist to do. nobody felt comfortable making a decision. >> middle health issues both in pregnancy and following pregnancy -- we said earlier on that the instance is about 10%- 15%. the risk of suicide in pregnancy is extraordinarily low. we all know that women can suffer from post natal depression and the risk of suicide still there following pregnancy. it is my belief that the risk of suicide can increase a little bit postnatal day. that is a question you could -- post-natally. that
97 Views
IN COLLECTIONS
CSPAN Television Archive
Television Archive  Television Archive News Search Service
Television Archive News Search Service 
Uploaded by TV Archive on

 Live Music Archive
Live Music Archive Librivox Free Audio
Librivox Free Audio Metropolitan Museum
Metropolitan Museum Cleveland Museum of Art
Cleveland Museum of Art Internet Arcade
Internet Arcade Console Living Room
Console Living Room Books to Borrow
Books to Borrow Open Library
Open Library TV News
TV News Understanding 9/11
Understanding 9/11